
Did you know the average person spends a whopping 26 years asleep? That’s a third of our lives cozied up in bed! From an evolutionary standpoint, sleep is essential for all mammals, including us humans.
Interestingly, humans are the only mammals that voluntarily delay sleep, yet it’s far from a luxury—it’s the cornerstone of thriving health!
For type 1 diabetes caregivers, sleep is a crucial tool in managing the challenges diabetes presents. However, sound sleep is often difficult to come by, plagued by fears of low blood sugar and the relentless buzz of CGM alarms. But it doesn’t have to be this way.
In today’s post, let’s explore five essential sleep strategies for type 1 diabetes caregivers. Implementing just one will help ease fears and promote restful sleep. Let’s dive in!
Strategy #1: Honor your body’s natural rhythms
Did you know the body operates on a 24-hour cycle called the circadian rhythm? The circadian rhythm is our body’s internal clock. Having an automatic, internal clock ensures certain processes are optimized throughout a 24-hour period.
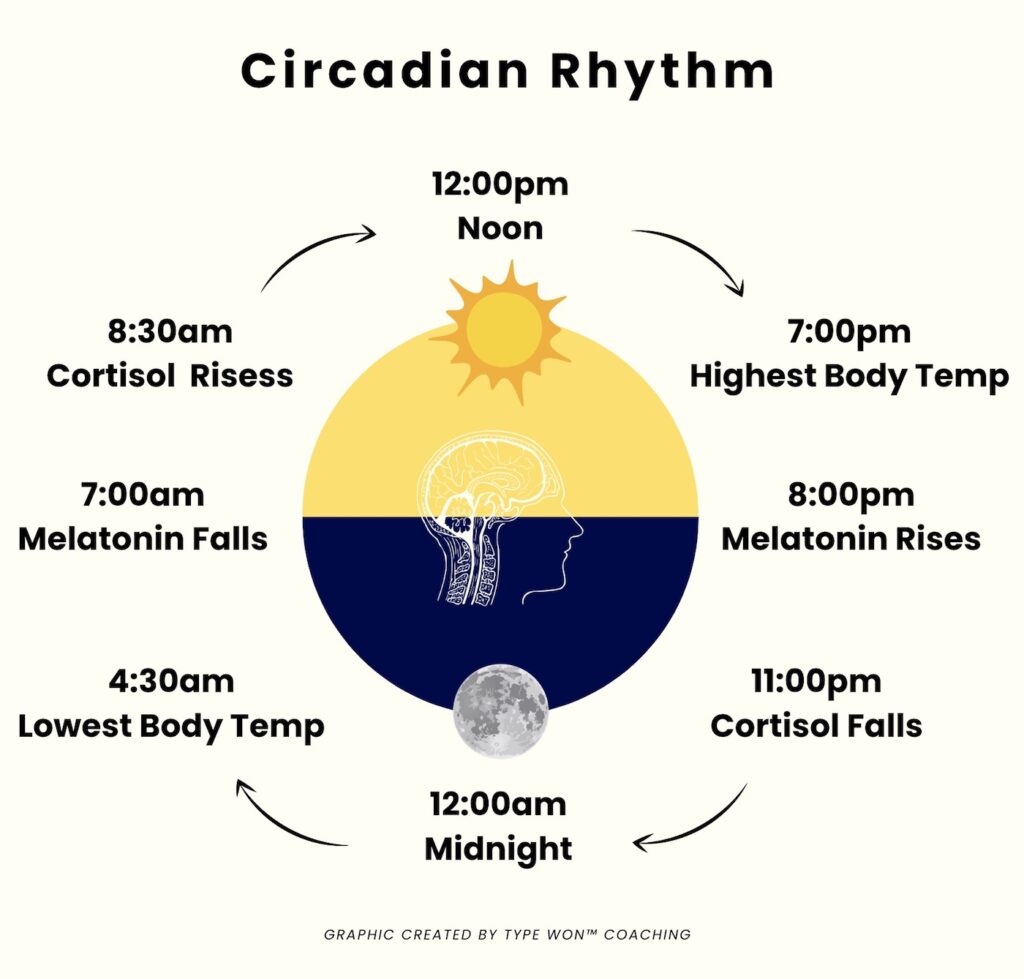
Our sleep-wake cycle is deeply influenced by our circadian rhythm. As the sun sets, the brain’s pineal gland releases melatonin, signaling the body to relax and prepare for sleep.
Upon waking, melatonin levels decrease, preventing grogginess during the day, while cortisol (the stress hormone) peaks around 9:00am, helping us wake up for the day.

Unfortunately, sleep suffers when cortisol levels remain high. Elevated cortisol signals to your body to remain in fight or flight versus rest and digest.
With a solid understanding of the circadian rhythm, it’s important to respect our body’s internal clock. Aim to go to bed and wake at the same time each day. This will help your body get into a natural rhythm.
Strategy #2: Embrace a relaxing bedtime routine
Just as we prioritize consistent bedtime routines for our children, why not extend the same luxury to ourselves as adults? Too often, we skip winding down and jump straight from screen time to bed, making it difficult for our bodies to relax.
Research confirms that establishing a bedtime routine improves sleep quality, regulates our internal clock, reduces cortisol, boosts melatonin, and allows our minds to rest.
I encourage you to harness your creativity when brainstorming supportive sleep strategies for diabetes. Whether it’s reading in bed (by yourself or with your kiddos), taking a relaxing bath, meditating, or indulging in a calming skincare routine, find what works best for you! And if you’re looking for more self-care inspiration, check out my previous post here.

Strategy #3: Establish boundaries with electronics
When it comes to sound sleep, it’s important to establish boundaries with our electronics. While watching TV or scrolling Instagram may feel relaxing, it puts a significant strain on our brains. In fact, a 2019 study found that excessive TV time can lead to cognitive decline in language and memory. Additionally, TV takes time away from other cognitive stimulating activities like reading or drawing.
It’s also important to remember that the blue light emitted from electronics disrupts sleep patterns. While natural during the day, blue light exposure at night confuses our internal clocks. It signals to our bodies to increase the level of cortisol, so instead of winding down, we’re revving our systems up.
Life is meant to be enjoyed, so when it comes to electronics the key is finding balance. Can you enjoy just one TV episode instead of four or five? Or consider using blue light blocking glasses, such as my favorite found here.

Strategy #4: Create a supportive sleep environment
Creating a relaxing sleep environment is crucial for our well-being. When you step into your bedroom, how do you want to feel? For me, I want my bedroom to be a space of tranquility and calm.
Therefore, clothes are put away, surfaces are free of clutter, lights are dimmed and salt lamps are on to create a serene vibe.
Similarly, when considering diabetes care, evaluating the bedroom’s role in supporting your T1D warrior is paramount. Is it optimized for both sleep and diabetes management? Are essential supplies readily accessible?
In my husband’s case, it’s really important his phone is easily accessible to check blood sugar. You’ll find his phone positioned on the bedside table, plugged in and charging. We also ensure low blood sugar snacks, such as glucose tablets, are close-at-hand.
Being prepared on the front-end helps prevent fumbling in the dark… never fun! With a little preparation and organization before bed, he can easily and seamlessly reach for his CGM, make adjustments, and fall back asleep.
I encourage you to take inventory of your current bedroom set-up. What changes can be made to ensure your sleep environment is supportive of diabetes care?

Strategy #5: Support your peace of mind
On more difficult nights, identify how you can support your peace of mind. If you’ve been up helping your T1D warrior, it’s normal to have trouble falling back to sleep. Rather than getting frustrated or sitting with racing thoughts, can you plug into a peaceful meditation to help you fall back to sleep?
Or do you need to journal to capture all your fears and concerns on paper? Maybe you need to wake your partner for extra support. Remember to honor your emotions, and never be afraid to ask for help.
Let’s recap
Sleep is the bedrock to thriving health, and it’s a powerful influence along the diabetes journey. Luckily, there are many supportive sleep strategies for type 1 diabetes caregivers.
Creating a relaxing environment, organizing diabetes supplies and getting to bed at a decent hour help foster restorative sleep. So, what is one action you will take today to prioritize sound sleep?
And if you’re looking for more sleep strategies for type 1 diabetes caregivers, a coaching partnership is here to help! To learn more please contact me at hello@typewoncoaching.com or via this link.
Until next time, sending you and your family so much love,
Allee
Leave a comment +